Situational analysis of nursing professionals to develop a strategic plan in a highly complex hospital
DOI:
https://doi.org/10.23938/ASSN.1116Keywords:
Job Satisfaction, Burnout. Professional, Nursing Staff, Work Engagement, Nursing CareAbstract
Background. This study aims to describe the emotional state, motivation, and satisfaction of nursing staff in order to design a management strategy to prevent burnout.
Methodology. A three-phase, cross-sectional study was conducted between December 2021 and February 2023 in a high-complexity hospital. Participants included professionals under the Nursing Directorate (nursing, physiotherapy, occupational therapy, auxiliary nursing care technician, and pharmacy auxiliary technicians) with ≥2 years of employment and ≥2 months in their current department. Data were collected using 65 items covering sociodemographic variables, willingness to choose the same profession again, emotional state (EVEA questionnaire), job satisfaction (Font-Roja questionnaire), and knowledge of internal organizational factors (self-designed questionnaire).
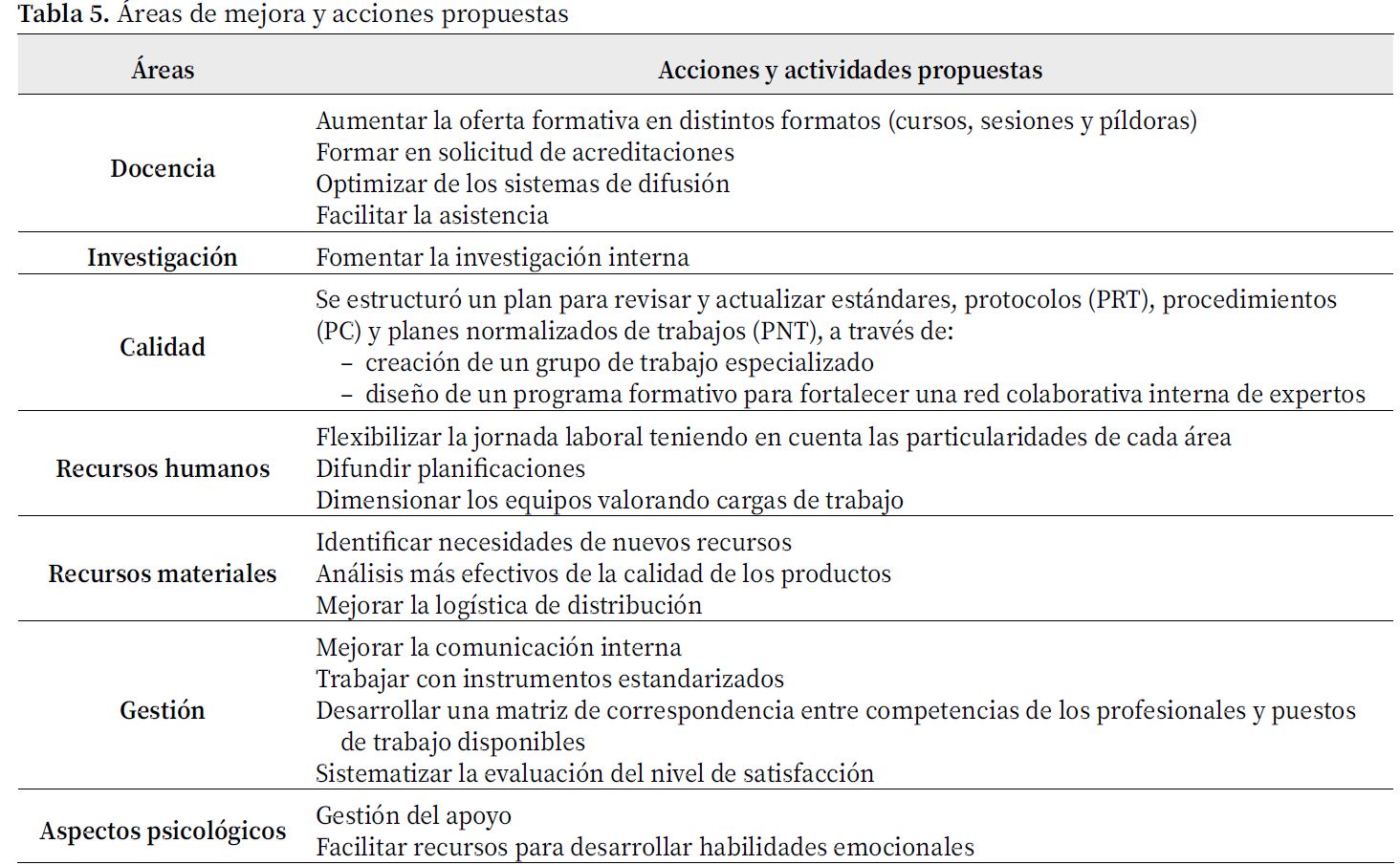
Results. A total of 596 professionals participated; 56% had ≤10 years of experience in the hospital and 59% would choose the same profession again. The EVEA questionnaire revealed high levels of anger, anxiety, and sadness. Font Roja scores indicated fatigue and difficulty disconnecting from work in 78% of participants. Although 70% responded good supervisor communication, limited leadership was identified. Associations were found between work shift, professional category, and emotional and satisfaction variables. Seven areas for improvement were identified to guide a strategic plan, with the most frequent demands related to human resources management.
Conclusions. Nurses exhibits higher burnout levels than physiotherapists, emphasizing the need for targeted interventions. Strengthening supervisory leadership and implementing tailored management strategies can align institutional goals with the expressed need of care teams.
Downloads
References
1. Alonso Carracedo P, Aguilera Duque AM. Relación entre satisfacción laboral y clima organizacional: Un metaanálisis. Apunt Psicol 2021; 39(1): 27-37.
2. Larsman P, Pousette A, Törner M. The impact of a climate of perceived organizational support on nurses' well-being and healthcare-unit performance: A longitudinal questionnaire study. J Adv Nurs 2024; 80: 4921-4932. http://doi.org/10.1111/jan.16188
3. Pérez Díaz J, Ramiro Fariñas D, Aceituno Nieto P, Escudero Martínez J, Bueno López C, Castillo Belmonte AB, et al. Un perfil de las personas mayores en España, 2023. Indicadores estadísticos básicos. Madrid: CCHS-CSIC; 2023. Informes Envejecimiento en red nº 30. https://envejecimientoenred.csic.es/wp-content/uploads/2023/10/enred-indicadoresbasicos2023.pdf
4. Esmaeilzadeh P. Challenges and strategies for wide-scale artificial intelligence (AI) deployment in healthcare practices: A perspective for healthcare organizations. Artif Intell Med 2024; 151: 102861. http://doi.org/10.1016/j.artmed.2024.102861
5. Sarría-Santamera A, Yeskendir A, Maulenkul T, Orazumbekova B, Gaipov A, Imaz-Iglesia I et al. Population health and health services: Old challenges and new realities in the COVID-19 era. Int J Environ Res Public Health 2021; 18(4): 1658. http://doi.org/10.3390/ijerph18041658
6. Instituto Nacional de Estadistica. Estadística de profesionales sanitarios colegiados. Año 2024. https://www.ine.es/dyngs/INEbase/es/operacion.htm?c=Estadistica_C&cid=1254736176781&menu=ultiDatos&idp=1254735573175
7. Aiken LH, Sloane DM, Bruyneel L, Van den Heede K, Griffiths P, Busse R et al. Nurse staffing and education and hospital mortality in nine European countries: A retrospective observational study. Lancet 2014; 383(9931): 1824-1830. http://doi.org/10.1016/s0140-6736(13)62631-8.
8. Al-Ghraiybah T, Lago L, Fernandez R, Sim J. Effects of the nursing practice environment, nurse staffing, patient surveillance and escalation of care on patient mortality: A multi-source quantitative study. Int J Nurs Stud 2024: 156: 104777. http://doi.org/10.1016/j.ijnurstu.2024.104777
9. Rochefort CM, Beauchamp ME, Audet LA, Abrahamowicz M, Bourgault P. Associations of 4 nurse staffing practices with hospital mortality. Med Care 2020; 58(10): 912-918. http://doi.org/10.1097/mlr.0000000000001397
10. Escobar-Aguilar G, Gómez-García T, Ignacio-García E, Rodríguez-Escobar J, Moreno-Casbas T, Fuentelsaz-Gallego C et al. Entorno laboral y seguridad del paciente: Comparación de datos entre los estudios SENECA y RN4CAST. Enferm Clin 2013; 23(3): 103-113. Spanish. http://doi.org/10.1016/j.enfcli.2013.03.005
11. Mir-Tabar A, Pardo-Herrera L, Goñi-Blanco A, Martínez-Rodríguez MT, Goñi-Viguria R. Patient satisfaction with nursing care in an Intensive Care Unit measured through the Nursing Intensive-Care Satisfaction Scale (NICSS). Enferm Intensiva (Engl Ed) 2024; 35(3): 201-212. http://doi.org/10.1016/j.enfie.2023.10.004
12. Palese A, Gonella S, Fontanive A, Guarnier A, Barelli P, Zambiasi P et al. The degree of satisfaction of in-hospital medical patients with nursing care and predictors of dissatisfaction: Findings from a secondary analysis. Scand J Caring Sci 2017; 31(4): 768-778. http://doi.org/10.1111/scs.12396
13. Lombardo C, Mento C, De Stefano R, Infortuna C, Iannuzzo F, Materia N et al. Job satisfaction in the health professions: The role of affective temperaments. Work 2023; 75(3): 1001-1007. http://doi.org/10.3233/WOR-220164.
14. Ge MW, Hu FH, Jia YJ, Tang W, Zhang WQ, Chen HL. Global prevalence of nursing burnout syndrome and temporal trends for the last 10 years: A meta-analysis of 94 studies covering over 30 countries. J Clin Nurs 2023; 32(17-18): 5836-5854. http://doi.org/10.1111/jocn.16708
15. Burmeister EA, Kalisch BJ, Xie B, Doumit MAA, Lee E, Ferraresion A et al. Determinants of nurse absenteeism and intent to leave: An international study. J Nurs Manag 2019; 27(1): 143-153. http://doi.org/10.1111/jonm.12659
16. Ministerio de Sanidad. Sistema de Notificación y Aprendizaje para la Seguridad del Paciente (SiNASP): Incidentes de seguridad notificados en 2023. Informes, estudios e investigación. Madrid: Ministerio de Sanidad; 2025. NIPO: 133-21-084-6.
17. Vermeir P, Blot S, Degroote S, Vandijck D, MarimanA, Vanacker T et al. Communication satisfaction and job satisfaction among critical care nurses and their impact on burnout and intention to leave: A questionnaire study. Intensive Crit Care Nurs 2018; 48: 21-27. http://doi.org/10.1016/j.iccn.2018.07.001
18. Ellis LA, Tran Y, Pomare C, Long JC, Churruca K, Saba M et al. Hospital organizational change: The importance of teamwork culture, communication, and change readiness. Front Public Health 2023; 11: 1089252. http://doi.org/10.3389/fpubh.2023.1089252
19. Zhang XJ, Song Y, Jiang T, Ding N, Shi TY. Interventions to reduce burnout of physicians and nurses: An overview of systematic reviews and meta-analyses. Medicine (Baltimore) 2020 26; 99(26): e20992. http://doi.org/10.1097/md.0000000000020992.17
20. Daugherty Biddison EL, Paine L, Murakami P, Herzke C, Weaver SJ. Associations between safty culture and employee engagement over time: A retrospective analysis. BMJ Qul Saf 2016; 25: 31-37. http://doi.org/10.1136/bmjqs-2014-003910
21. Cobarsí Morales J, Calvet Liñan L, Segundo Martín E. Muertes por COVID-19 en España durante la ‘primera ola’: Datos cuantitativos y su tratamiento periodístico. Rev Gen Inf Doc 2022; 32(1): 61-91. http://doi.org/10.5209/rgid.82948
22. Sánchez-Romero S, Ruiz-Fernández MD, Fernández-Medina IM, Del Mar Jiménez-Lasserrotte M, Del Rocío Ramos-Márquez M, Ortega-Galán ÁM. Experiences of suffering among nursing professionals during the COVID-19 pandemic: A descriptive qualitative study. Appl Nurs Res 2022; 66: 151603. http://doi.org/10.1016/j.apnr.2022.151603.
23. Blanco-Daza M, de la Vieja-Soriano M, Macip-Belmonte S, Tercero-Cano MDC. Trastorno de estrés postraumático en enfermeras durante la pandemia de COVID-19. Enferm Clin. 2022; 32(2): 92-102. http://doi.org/10.1016/j.enfcli.2021.10.015.
24. Vázquez Caubet JC, Sánchez-Arcilla Conejo I, Caso Pita C, Pacheco Tabuenca T. Prevención del desgaste profesional en los centros sanitarios del Servicio Madrileño de Salud. Madrid: Subdirección de Humanización de la Asistencia Sanitaria, Consejería de Sanidad; 2019. http://www.madrid.org/bvirtual/BVCM020304.pdf
25. Sanz J. Un instrumento para evaluar la eficacia de los procedimientos de inducción de estado de ánimo: La “escala de valoración del estado de ánimo” (EVEA). Análisis y Modificación de Conducta 2001; 27(111): 71-110. https://docta.ucm.es/rest/api/core/bitstreams/1b8af7e9-8c99-4c11-b903-0b400d1a4e06/content
26. Aranaz Andrés JM, Mira J. Cuestionario Font Roja. Un instrumento de medida de la satisfacción en el medio hospitalario. Todo Hosp 1988; 52: 63-68
27. Bell M, Sheridan A. How organisational commitment influences nurses' intention to stay in nursing throughout their career. Int J Nurs Stud Adv 2020; 2: 100007. http://doi.org/10.1016/j.ijnsa.2020.100007
28. Arimon-Pagès E, Torres-Puig-Gros J, Fernández-Ortega P, Canela-Soler J. Emotional impact and compassion fatigue in oncology nurses: Results of a multicentre study. Eur J Oncol Nurs 2019; 43: 101666. http://doi.org/10.1016/j.ejon.2019.09.007
29. Cummings GG, Tate K, Lee S, Wong CA, Paananen T, Micaroni SPM et al. Leadership styles and outcome patterns for the nursing workforce and work environment: A systematic review. Int J Nurs Stud 2018; 85: 19-60. http://doi.org/10.1016/j.ijnurstu.2018.04.016
30. García-Vivar C, Ferraz-Torres M, Escalada-Hernández P, Soto-Ruiz N. Intención de abandono de la profesión enfermera por salud mental en Navarra (España) durante la pandemia de COVID-19. An Sist Sanit Navar 2025; 48(1): e1110. http://doi.org/10.23938/ASSN.1110
31. Butler M, Schultz TJ, Halligan P, Sheridan A, Kinsman L, Rotter T, Beaumier J, Kelly RG, Drennan J. Hospital nurse-staffing models and patient- and staff-related outcomes. Cochrane Database Syst Rev 2019; 4(4): CD007019. http://doi.org/10.1002/14651858.CD007019
32. Lin RT, Lin YT, Hsia YF, Kuo CC. Long working hours and burnout in health care workers: Non- linear dose-response relationship and the effect mediated by sleeping hours-A cross-sectional study. J Occup Health 2021; 63(1): e12228. http://doi.org/10.1002/1348-9585.12228
33. Griffiths P, Saville C, Ball J, Dall'Ora C, Meredith P, Turner L, Jones J. Costs and cost- effectiveness of improved nurse staffing levels and skill mix in acute hospitals: A systematic review. Int J Nurs Stud 2023; 147: 104601. http://doi.org/10.1016/j.ijnurstu.2023.104601
34. Sexton JB, Adair KC, Leonard MW, Frankel TC, Proulx J, Watson SR et al. Providing feedback following Leadership WalkRounds is associetad with better patient safety cultura, hihger employee engagement and lower burnout. BMJ Qual Saf 2018; 27: 261-271. http://doi.org/10.1136/bmjqs- 2016-006399
35. Larsman P, Pousette A, Törner M. The impact of a climate of perceived organizational support on nurses' well-being and healthcare-unit performance: A longitudinal questionnaire study. J Adv Nurs 2024; 80(12): 4921-4932. http://doi.org/10.1111/jan.16188
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2025 Anales del Sistema Sanitario de Navarra

This work is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License.
La revista Anales del Sistema Sanitario de Navarra es publicada por el Departamento de Salud del Gobierno de Navarra (España), quien conserva los derechos patrimoniales (copyright ) sobre el artículo publicado y favorece y permite la difusión del mismo bajo licencia Creative Commons Reconocimiento-CompartirIgual 4.0 Internacional (CC BY-SA 4.0). Esta licencia permite copiar, usar, difundir, transmitir y exponer públicamente el artículo, siempre que siempre que se cite la autoría y la publicación inicial en Anales del Sistema Sanitario de Navarra, y se distinga la existencia de esta licencia de uso.







