Sentido de coherencia en mujeres lactantes: una revisión de alcance
DOI:
https://doi.org/10.23938/ASSN.1064Palabras clave:
Sentido de coherencia, Lactancia materna, Salud materno infantil, Adaptación psicológicaResumen
Fundamento. El establecimiento de la lactancia materna puede resultar una situación potencialmente estresante. El objetivo del estudio es analizar el sentido de coherencia en mujeres lactantes, establecer los recursos generales de resistencia que lo modulan, y determinar las intervenciones profesionales que lo promueven.
Metodología. Se incluyeron estudios en inglés, español o portugués, que evaluaran el sentido de coherencia de las mujeres lactantes, localizados en las bases de datos PubMed, PsycINFO, ScienceDirect y CINAHL entre marzo y mayo de 2023. La calidad de los estudios y el riesgo de sesgo se evaluaron siguiendo los criterios ICROMS y STROBE.
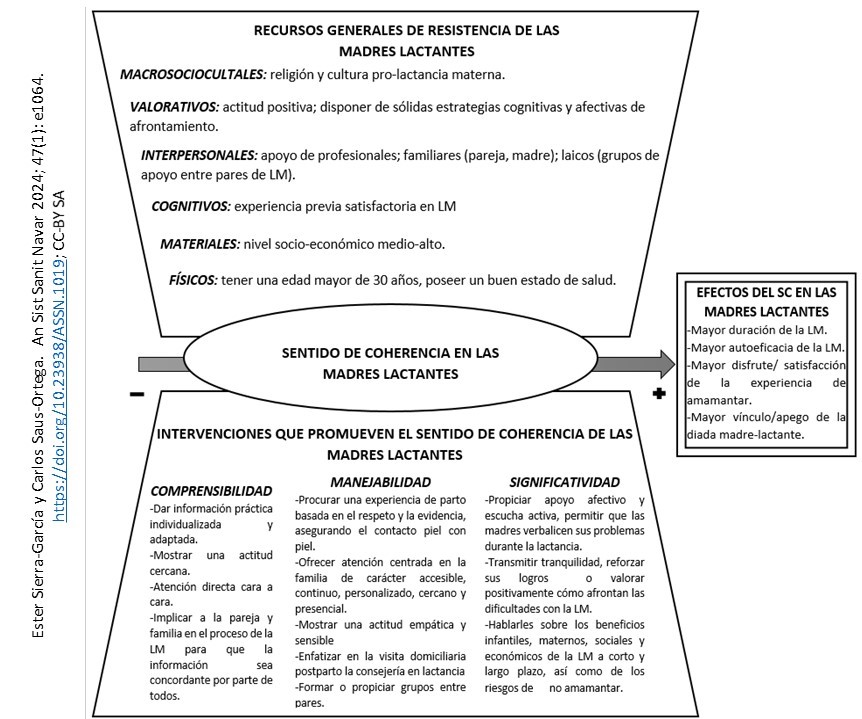
Resultados. Se identificaron 316 registros, de los que se incluyeron un total de ocho estudios, tres cualitativos y cinco cuantitativos, todos con calidad suficiente. Un alto nivel de sentido de coherencia materno se relacionó con mayor duración, autoeficacia y disfrute de la experiencia de lactancia, y mayor apego. Los principales recursos generales de resistencia fueron percibir apoyo social, especialmente de parejas, madres y personal sanitario, además de experiencia previa positiva y una actitud positiva. Las intervenciones que favorecieron el sentido de coherencia fueron las relacionadas con un apoyo profesional estrecho, empático, personalizado, integral y centrado en la familia.
Conclusiones. La determinación del nivel de sentido de coherencia en madres lactantes puede ayudar a identificar a mujeres con mayor riesgo de destete temprano, y a establecer estrategias de intervención profesional que mejoren la experiencia de lactancia materna
Descargas
Citas
MOSCA F, GIANNÌ ML. Human milk: composition and health benefits. Pediatr Medica E Chir Med Surg Pediatr 2017; 39(2): 155. https://doi.org/10.4081/pmc.2017.155
PATEL R, OKEN E, BOGDANOVICH N, MATUSH L, SEVKOVSKAYA Z, CHALMERS B et al. Cohort profile: The promotion of Breastfeeding Intervention Trial (PROBIT). Int J Epidemiol 2014; 43(3): 679-690. https://doi.org/10.1093/ije/dyt003
SHAMIR R. The benefits of breast feeding. Nestle Nutr Inst Workshop Ser 2016; 86: 67-76. https://doi.org/10.1159/000442724
WALTERS DD, PHAN LTH, MATHISEN R. The cost of not breastfeeding: global results from a new tool. Health Policy Plan 2019; 34(6): 407-417. https://doi.org/10.1093/heapol/czz050
BENJAMIN NEELON SE, STROO M, MAYHEW M, MASELKO J, HOYO C. Correlation between maternal and infant cortisol varies by breastfeeding status. Infant Behav Dev 2015; 40: 252-258. https://doi.org/10.1016/j.infbeh.2015.06.005
GERTOSIO C, MEAZZA C, PAGANI S, BOZZOLA M. Breastfeeding and its gamut of benefits. Minerva Pediatr 2016; 68(3): 201-212.
KROL KM, GROSSMANN T. Psychological effects of breastfeeding on children and mothers. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz 2018; 61(8): 977-985. https://doi.org/10.1007/s00103-018-2769-0
United Nations Children’s Fund (UNICEF), World Health Organization (WHO). Global breastfeeding scorecard 2022: Protecting breastfeeding through further investments and policy actions. Ginebra: OMS, 2022. https://www.who.int/publications-detail-redirect/WHO-HEP-NFS-22.6
AREIA J, PORTO T, SILVA Á, BALDOINO L, ARAÚJO R, MARTINS V et al. As principais motivações elencadas para o desmame precoce por lactantes adultas: revisão integrativa da literatura. Rev Eletrônica Acervo Saúde 2020; e2568. http://doi.org/10.25248/reas.e2568.2020
ROLLINS NC, BHANDARI N, HAJEEBHOY N, HORTON S, LUTTER CK, MARTINES JC et al. Why invest, and what it will take to improve breastfeeding practices? The Lancet 2016; 387(10017): 491-504. https://doi.org/10.1016/s0140-6736(15)01044-2
BROWN A, RANCE J, BENNETT P. Understanding the relationship between breastfeeding and postnatal depression: the role of pain and physical difficulties. J Adv Nurs 2016; 72(2): 273-282. https://doi.org/10.1111%2Fjan.12832
PALMÉR L. Previous breastfeeding difficulties: an existential breastfeeding trauma with two intertwined pathways for future breastfeeding—fear and longing. Int J Qual Stud Health Well-Being 2019; 14(1): 1588034. https://doi.org/10.1080%2F17482631.2019.1588034
BROWN CRL, DODDS L, LEGGE A, BRYANTON J, SEMENIC S. Factors influencing the reasons why mothers stop breastfeeding. Can J Public Health 2014; 105(3): e179-85. https://doi.org/10.17269/cjph.105.4244
SILVA CS, LIMA MC, SEQUEIRA-DE-ANDRADE LAS, OLIVEIRA JS, MONTEIRO JS, LIMA NMS et al. Association between postpartum depression and the practice of exclusive breastfeeding in the first three months of life. J Pediatr (Rio J) 2017; 93(4): 356-364. https://doi.org/10.1016/j.jped.2016.08.005
COOK N, AYERS S, HORSCH A. Maternal posttraumatic stress disorder during the perinatal period and child outcomes: A systematic review. J Affect Disord 2018; 225: 18-31. https://doi.org/10.1016/j.jad.2017.07.045
FALLON V, GROVES R, HALFORD JCG, BENNETT KM, HARROLD JA. Postpartum anxiety and infant-feeding outcomes. J Hum Lact Off J Int Lact Consult Assoc 2016; 32(4): 740-758. https://doi.org/10.1177/0890334416662241
BEAKE S, BICK D, NARRACOTT C, CHANG YS. Interventions for women who have a caesarean birth to increase uptake and duration of breastfeeding: A systematic review. Matern Child Nutr 2017; 13(4): e12390. https://doi.org/10.1111/mcn.12390
PATEL S, PATEL S. The effectiveness of lactation consultants and lactation counselors on breastfeeding outcomes. J Hum Lact Off 2016; 32(3): 530-541. https://doi.org/10.1177/0890334415618668
MCFADDEN A, GAVINE A, RENFREW MJ, WADE A, BUCHANAN P, TAYLOR JL et al. Support for healthy breastfeeding mothers with healthy term babies. Cochrane Database Syst Rev 2017; 2: CD001141. https://doi.org/10.1002/14651858.cd001141.pub5
RIVERA DE LOS SANTOS F, RAMOS VALVERDE P, MORENO RODRÍGUEZ C, HERNÁN GARCÍA M. Análisis del modelo salutogénico en España: aplicación en salud pública e implicaciones para el modelo de activos en salud. Rev Esp Salud Pública 2011; 85(2): 129-139. https://scielo.isciii.es/pdf/resp/v85n2/02_colaboracion1.pdf
ANTONOVSKY A. Sense of coherence scale. San Francisco: Jossey-Bass, 1979.
ANTONOVSKY A. Health, stress and coping. Unraveling the mystery of health: How people manage stress and stay well. San Francisco: Jossey-Bass, 1979.
ANTONOVSKY A. The structure and properties of the sense of coherence scale. Soc Sci Med. 1993; 36(6): 725-733. https://doi.org/10.1016/0277-9536(93)90033-z
POURSALEHI R, NAJIMI A, TAHANI B. Effect of sense of coherence on oral health behavior and status: A systematic review and meta-analysis. J Educ Health Promot 2021; 10: 361. https://doi.org/10.4103/jehp.jehp_1350_20
CHANG YS, BEAKE S, KAM J, LOK KYW, BICK D. Views and experiences of women, peer supporters and healthcare professionals on breastfeeding peer support: A systematic review of qualitative studies. Midwifery 2022; 108: 103299. https://doi.org/10.1016/j.midw.2022.103299
FLACKING R, TANDBERG BS, NIELA-VILÉN H, JÓNSDÓTTIR RB, JONAS W, EWALD U et al. Positive breastfeeding experiences and facilitators in mothers of preterm and low birthweight infants: a meta-ethnographic review. Int Breastfeed J 2021; 16(1): 88. https://doi.org/10.1186/s13006-021-00435-8
DA SILVA TANGANHITO D, BICK D, CHANG YS. Breastfeeding experiences and perspectives among women with postnatal depression: A qualitative evidence synthesis. Women Birth 2020; 33(3): 231-239. https://doi.org/10.1016/j.wombi.2019.05.012
KARAÇAM Z, SAĞLIK M. Breastfeeding problems and interventions performed on problems: systematic review based on studies made in Turkey. Turk Pediatri Ars 2018; 53(3): 134-148. https://doi.org/10.5152/turkpediatriars.2018.6350
DODGSON JE. What is a state of the science research review? J Hum Lact 2023; 39(1): 23-9. https://doi.org/10.1177/08903344221142263
PETERS MDJ, MCINERNEY P, MUNN Z, TRICCO AC, KHALIL H. Chapter 11: Scoping reviews. En AROMATARIS E, MUNN Z, editores. JBI manual for evidence synthesis. JBI, 2020; 406-451. https://doi.org/10.46658/JBIMES-20-12
Medical Subject Headings 2021. MeSH Browser. Consultado el 10 de septiembre de 2021. https://meshb.nlm.nih.gov/
Organización Mundial de la Salud, editor. Indicadores para evaluar las prácticas de alimentación del lactante y del niño pequeño: conclusiones de la reunión de consenso llevada a cabo del 6 al 8 de noviembre de 2007 en Washington, DC, EEUU. Ginebra: OMS, 2009. https://iris.who.int/bitstream/handle/10665/44156/9789243596662_spa.pdf?sequence=1
SAWMA T, SANJAB Y. The association between sense of coherence and quality of life: a cross-sectional study in a sample of patients on hemodialysis. BMC Psychol 2022; 10(1): 100. https://doi.org/10.1186/s40359-022-00805-9
MÁRQUEZ-PALACIOS JH, YANEZ-PEÑÚÑURI LY, SALAZAR-ESTRADA JG. Relationship between sense of coherence and diabetes mellitus: a systematic review. Cienc Saude Coletiva 2020; 25(10): 3955-3967. https://doi.org/10.1590/1413-812320202510.34312018
BRINGSVOR HB, LANGELAND E, OFTEDAL BF, SKAUG K, ASSMUS J, BENTSEN SB. Effects of a COPD self-management support intervention: a randomized controlled trial. Int J Chron Obstruct Pulmon Dis 2018; 13: 3677-3688. https://doi.org/10.2147/copd.s181005
MIKUTTA C, SCHMID JJ, EHLERT U. Resilience and post-traumatic stress disorder in the Swiss Alpine Rescue Association. Front Psychiatry 2022; 13. https://doi.org/10.3389/fpsyt.2022.780498
SCHWAAB L, GEBHARDT N, FRIEDERICH HC, NIKENDEI C. Climate change related depression, anxiety and stress symptoms perceived by medical students. Int J Environ Res Public Health 2022; 19 (15): 9142. https://doi.org/10.3390/ijerph19159142
YAGHOOBI H, FARAHANI AS, ROHANI C. The role of the mothers’ sense of coherence in predicting dental caries risk in children. Community Dent Health 2022; 39(3): 206-210. https://doi.org/10.1922/cdh_00112yaghoobi05
GOMES MC, PERAZZO MF, NEVES ÉT, MARTINS CC, PAIVA SM, GRANVILLE-GARCIA AF. Oral problems and self-confidence in preschool children. Braz Dent J 2017; 28(4): 523-530. https://doi.org/10.1590/0103-6440201601295
DA COSTA AC, RODRIGUES FS, DA FONTE PP, ROSENBLATT A, INNES NPT, HEIMER MV. Influence of sense of coherence on adolescents’ self-perceived dental aesthetics; a cross-sectional study. BMC Oral Health 2017; 17(1): 117. https://doi.org/10.1186/s12903-017-0405-2
ERIKSSON M, LINDSTRÖM B. Validity of Antonovsky’s sense of coherence scale: a systematic review. J Epidemiol Community Health 2005; 59(6): 460-466. https://doi.org/10.1136/jech.2003.018085
ZINGG W, CASTRO-SANCHEZ E, SECCI FV, EDWARDS R, DRUMRIGHT LN, SEVDALIS N et al. Innovative tools for quality assessment: integrated quality criteria for review of multiple study designs (ICROMS). Public Health 2016; 133: 19-37. https://doi.org/10.1016/j.puhe.2015.10.012
VON ELM E, ALTMAN DG, EGGER M, POCOCK SJ, GØTZSCHE PC, VANDENBROUCKE JP. Declaración de la Iniciativa STROBE (Strengthening the Reporting of Observational studies in Epidemiology): directrices para la comunicación de estudios observacionales. Gac Sanit 2008; 22(2): 144-150. https://doi.org/10.1157/13119325
CORTELO FM, MARBA STM, CORTELLAZZI KL, AMBROSANO GMB, GUERRA LM, ALMEIDA ACG et al. Women’s sense of coherence and its association with early weaning. J Pediatr (Rio J) 2018; 94(6): 624-629. https://doi.org/10.1016/j.jped.2017.08.007
KOLANEN H, VÄLIMÄKI T, VEHVILÄINEN-JULKUNEN K. Breastfeeding among somali mother’s living in finland under salutogenic approach. Int J Caring Sci 2016; 9. http://www.internationaljournalofcaringsciences.org/docs/1_Vehvilainen-Julkunen_original_9_2.pdf
THOMSON G, DYKES F. Women’s sense of coherence related to their infant feeding experiences. Matern Child Nutr 2011; 7(2): 160-174. https://doi.org/10.1111/j.1740-8709.2010.00251.x
BYROM A, THOMSON G, DOORIS M, DYKES F. UNICEF UK Baby Friendly Initiative: Providing, receiving and leading infant feeding care in a hospital maternity setting-A critical ethnography. Matern Child Nutr 2021; 17(2): e13114. https://doi.org/10.1111/mcn.13114
GRANBERG A, EKSTRÖM-BERGSTRÖM A, BÄCKSTRÖM C. First-Time mothers’ enjoyment of breastfeeding correlates with duration of breastfeeding, sense of coherence, and parental couple and child relation: a longitudinal swedish cohort study. Nurs Res Pract 2020; 2020: 8194389. https://doi.org/10.1155/2020/8194389
LINDEN K, BERG M, ADOLFSSON A, SPARUD-LUNDIN C. Well-being, diabetes management and breastfeeding in mothers with type 1 diabetes - An explorative analysis. Sex Reprod Healthc 2018; 15: 77-82. https://doi.org/10.1016/j.srhc.2017.12.004
PAVICIC BOSNJAK A, RUMBOLDT M, STANOJEVIC M, DENNIS CL. Psychometric assessment of the croatian version of the breastfeeding self-efficacy scale-short form. J Hum Lact 2012; 28(4): 565-569. https://doi.org/10.1177/0890334412456240
NAKATANI M, OBAYASHI Y, TANIMURA S, SHINKODA H. Breastfeeding self-efficacy of mothers with infants in the neonatal intensive care unit beyond one month from starting breastfeeding and the related factors. J Jpn Acad Nurs Sci 2020; 40: 168-176. http://doi.org/10.5630/jans.40.168
BRAUN-LEWENSOHN O, MAYER CH. Salutogenesis and coping: ways to overcome stress and conflict. Int J Environ Res Public Health 2020; 17(18): 6667. https://doi.org/10.3390/ijerph17186667
LÄNSIMIES H, PIETILÄ AM, HIETASOLA-HUSU S, KANGASNIEMI M. A systematic review of adolescents’ sense of coherence and health. Scand J Caring Sci 2017; 31(4): 651-661. https://doi.org/10.1111/scs.12402
DEL-PINO-CASADO R, ESPINOSA-MEDINA A, LÓPEZ-MARTÍNEZ C, ORGETA V. Sense of coherence, burden and mental health in caregiving: A systematic review and meta-analysis. J Affect Disord 2019; 242: 14-21. https://doi.org/10.1016/j.jad.2018.08.002
MITCHELL-BOX KM, BRAUN KL. Impact of male-partner-focused interventions on breastfeeding initiation, exclusivity, and continuation. J Hum Lact 2013; 29(4): 473-479. https://doi.org/10.1177/0890334413491833
STANEVA A, MORAWSKA A, BOGOSSIAN F, WITTKOWSKI A. Pregnancy-specific distress: the role of maternal sense of coherence and antenatal mothering orientations. J Ment Health 2016; 25(5): 387-394. https://doi.org/10.3109/09638237.2015.1101425
LIBERA A, DARMOCHWAL-KOLARZ D, OLESZCZUK J. Sense of coherence (SOC) and styles of coping with stress in women after premature delivery. Med Sci Monit 2007; 13(3): CR125-130.
PRADO CVC, FABBRO MRC, FERREIRA GI. Desmame precoce na perspectiva de puérperas: uma abordagem dialógica. Texto Contexto Enferm 2016; 25(2): 1-9.
ALDERDICE F, MCNEILL J, LYNN F. A systematic review of systematic reviews of interventions to improve maternal mental health and well-being. Midwifery 2013; 29(4): 389-399. https://doi.org/10.1016/j.midw.2012.05.010
SRINIVAS GL, BENSON M, WORLEY S, SCHULTE E. A clinic-based breastfeeding peer counselor intervention in an urban, low-income population: interaction with breastfeeding attitude. J Hum Lact 2015; 31(1): 120-128. https://doi.org/10.1177/0890334414548860
HUANG Y, OUYANG YQ, REDDING SR. Previous breastfeeding experience and its influence on breastfeeding outcomes in subsequent births: A systematic review. Women Birth 2019; 32(4): 303-309. https://doi.org/10.1016/j.wombi.2018.09.003
WAGNER S, KERSUZAN C, GOJARD S, TICHIT C, NICKLAUS S, THIERRY X et al. Breastfeeding initiation and duration in France: The importance of intergenerational and previous maternal breastfeeding experiences — results from the nationwide ELFE study. Midwifery 2019; 69: 67-75. https://doi.org/10.1016/j.midw.2018.10.020
MORSE H, BROWN A. The benefits, challenges and impacts of accessing social media group support for breastfeeding: A systematic review. Matern Child Nutr 2022; 18(4): e13399. https://doi.org/10.1111/mcn.13399
BIGELOW AE, MACLEAN K, PROCTOR J, MYATT T, GILLIS R, POWER M. Maternal sensitivity throughout infancy: continuity and relation to attachment security. Infant Behav Dev 2010; 33(1): 50-60. https://doi.org/10.1016/j.infbeh.2009.10.009
WOOD NK, WOODS NF, BLACKBURN ST, SANDERS EA. Interventions that enhance breastfeeding initiation, duration, and exclusivity: a systematic review. MCN Am J Matern Child Nurs 2016; 41(5): 299-307. https://doi.org/10.1097/nmc.0000000000000264
CHETWYND EM, WASSER HM, POOLE C. Breastfeeding support interventions by international board certified lactation consultants: a systemic review and meta-analysis. J Hum Lact 2019; 35(3): 424-440. https://doi.org/10.1177/0890334419851482
GRIFFIN LB, DING JJ, HAS P, AYALA N, KOLE-WHITE MB. Lactation consultation by an international board certified lactation consultant improves breastfeeding rates for mothers with gestational diabetes mellitus. J Hum Lact 2022; 38(1): 141-147. https://doi.org/10.1177/08903344211018622
GUALA A, BOSCARDINI L, VISENTIN R, ANGELLOTTI P, GRUGNI L, BARBAGLIA M et al. Skin-to-skin contact in cesarean birth and duration of breastfeeding: a cohort study. The Scientific World Journal 2017; 2017: 1940756. https://doi.org/10.1155/2017/1940756
KARIMI FZ, SADEGHI R, MALEKI-SAGHOONI N, KHADIVZADEH T. The effect of mother-infant skin to skin contact on success and duration of first breastfeeding: A systematic review and meta-analysis. Taiwan J Obstet Gynecol 2019; 58(1): 1-9. https://doi.org/10.1016/j.tjog.2018.11.002
ZAVALA-SOTO JO, HERNANDEZ-RIVERO L, TAPIA-FONLLEM C. Pro-lactation cesarean section: Immediate skin-to-skin contact and its influence on prolonged breastfeeding. Front Sociol 2022; 7: 908811. https://doi.org/10.3389/fsoc.2022.908811
SEKIZUKA-KAGAMI N, SHIMADA K, TABUCHI N, NAKAMURA H. Association between the sense of coherence 13-item version scale score of pregnant women in the second trimester of pregnancy and threatened premature birth. Environ Health Prev Med 2015; 20(2): 90-96. https://doi.org/10.1007/s12199-014-0436-0
FERGUSON S, BROWNE J, TAYLOR J, DAVIS D. Sense of coherence and women׳s birthing outcomes: A longitudinal survey. Midwifery 2016; 34: 158-165. https://doi.org/10.1016/j.midw.2015.11.017
FERGUSON S, DAVIS D. “I’m having a baby not a labour”: Sense of coherence and women’s attitudes towards labour and birth. Midwifery 2019; 79: 102529. https://doi.org/10.1016/j.midw.2019.102529
HABROE M, SCHMIDT L, EVALD HOLSTEIN B. Does childbirth after fertility treatment influence sense of coherence? A longitudinal study of 1,934 men and women. Acta Obstet Gynecol Scand 2007; 86(10): 1215-1221. https://doi.org/10.1080/00016340701619258
RODRÍGUEZ-GALLEGO I, LEON-LARIOS F, RUIZ-FERRÓN C, LOMAS-CAMPOS M DE LAS M. Evaluation of the impact of breastfeeding support groups in primary health centres in Andalusia, Spain: a study protocol for a cluster randomized controlled trial (GALMA project). BMC Public Health 2020; 20(1): 1129. https://doi.org/10.1186/s12889-020-09244-w
CHANG YS, BEAKE S, KAM J, LOK KYW, BICK D. Views and experiences of women, peer supporters and healthcare professionals on breastfeeding peer support: A systematic review of qualitative studies. Midwifery 2022; 108: 103299. https://doi.org/10.1016/j.midw.2022.103299
AHLBORG T, BERG S, LINDVIG J. Sense of coherence in first-time parents: a longitudinal study. Scand J Public Health 2013; 41(6): 623-629. https://doi.org/10.1177/1403494813484992
Publicado
Cómo citar
Número
Sección
Licencia

Esta obra está bajo una licencia internacional Creative Commons Atribución-CompartirIgual 4.0.
La revista Anales del Sistema Sanitario de Navarra es publicada por el Departamento de Salud del Gobierno de Navarra (España), quien conserva los derechos patrimoniales (copyright ) sobre el artículo publicado y favorece y permite la difusión del mismo bajo licencia Creative Commons Reconocimiento-CompartirIgual 4.0 Internacional (CC BY-SA 4.0). Esta licencia permite copiar, usar, difundir, transmitir y exponer públicamente el artículo, siempre que siempre que se cite la autoría y la publicación inicial en Anales del Sistema Sanitario de Navarra, y se distinga la existencia de esta licencia de uso.







