INTRODUCTION
Although the effects of the COVID-19 pandemic on mortality and economic activity have
been
the subject of steady media coverage, at the same time, the social and day-to-day aspects of this tragedy
are
frequently overlooked in public debates. As the pandemic spread, strict new measures and regulations were
introduced in a way that was both improvised and reactive in the context of a situation out of control.
Decisions had to be taken, and indeed were taken, based on insufficient knowledge about the disease and its
characteristics. One year later, the time has come to investigate how societies around the world initially
handled the pandemic and the extent to which it changed lives as a result. This paper focuses on the effects
of
the national lockdown in Spain (14 March 2020-21 June 2020) on perceived health. This initial regulation
lasted
only a few months and, although subsequent confinement measures were enacted, they did not affect the entire
country and were generally less restrictive regarding individual and collective human rights and civil
liberties. Thus, the social and individual consequences of those three months in Spring 2020 are of
particular
interest for three main reasons. First, the effects of the lockdown are not yet fully known, while the
disease
continues to evolve and spread, threatening the possibility of new closures. Therefore, the production of
knowledge related to the social implications of those epidemiological decisions is essential to inform
future
political decisions. Second, the consequences of the lockdown were profoundly divergent. Clearly, no one was
prepared for the situation, and in a sense, it was a shared experience, a hard time for everyone. A closer
look,
however, reveals how individual and family circumstances differed significantly, regarding both the material
conditions in which the lockdown was experienced and the challenges faced by each individual. In a context
of
pandemic, economic crisis and restrictions on mobility, micro-level differences related to resources and
limitations became even more important. This paper analyses the unequal consequences of those new routines
and
social conditions in the specific case of the population of Andalusia. Third, some effects of the lockdown
(such
as the effects on mental health) may have a longer time frame, and to treat these long-term effects we have
to
understand their origin and development.
The interest in perceived health lies in the capacity of this indicator to synthesize
the
objective circumstances of health (Shields & Shooshtari, 2001; Jindrová
& Labudová, 2020). This helps to not only determine subjective perceptions, but also obtain a
holistic
view of an individual’s situation in broader terms. Mood and context affect perceived health, as people
inevitably compare themselves with others and with their own memories. Recent research has studied the
effects
of the pandemic on perceived health in other countries, like France (Recchi et al.,
2020),
Germany (Ohlbrecht & Jellen, 2021) and Italy (Rossi et al., 2020),
showing how lockdown measures not only intensified previous social inequalities related to perceived health,
but
also created new fractures. However, most of these authors focus on particular groups, or on specific
behaviours
and emotions, without providing an overall assessment of the consequences of the lockdown for physical and
mental health. The results of this work, then, offer new insights for the study of perceived health and the
social consequences of COVID-19.
Using data from the 2020 Social Survey. Habits and Living Conditions of the
Andalusian
Population during the State of Alarm (IECA, 2020), this paper addresses three
specific
points: (1) how the lockdown has affected the general health perception of the Andalusian population and its
differential impacts by social group; (2) how demographic, socio-economic and residential conditions explain
health self-perception and whether these conditions have changed due to the pandemic; and (3) how specific
lockdown situations (such as changes in household composition, contact with COVID-19 and new economic
problems)
have affected the self-perception of health.
A BRIEF REVIEW OF THE IMPACT OF COVID-19 ON PERCEIVED HEALTH
Perceived health (also called self-reported or self-rated health) has been a
well-established topic in both public health and the sociology of health literature since the 1990s (Shields & Shooshtari, 2001). The spread of the topic in recent decades can be
attributed
to its ability to capture an impression of the overall objective health of people and predict mortality
and
illness well, in spite of its simplicity (Idler & Kasl, 1991; Idler
&
Kasl, 1995; Idler et al., 1990). At the same time, it can be used as a major
indicator
of a population’s well-being in a broader sense (Ohlbrecht & Jellen, 2021). Classic
studies on the topic - closer to medical approaches than sociological ones - focus on the relationship
between
perceived health and objective health and some demographic determinants, mainly sex and age (Idler & Kasl, 1995). However, the rapid incursion of the social sciences into health
issues, along with the ging popularization of the social determinants of health approach, have led
academics
to reframe the topic, resulting in an understanding of perceived health (as well as health in general) in
the
social context in which people live (WHO, 2008). Using this new framing, perceived
health has
become an outcome of the macro-social context, defined as the social, economic and cultural structures and
cycles in which people function. The micro-individual level was also reframed, paying greater attention to
social variables that explain perceived health such as education (Ross & Misky,
1999),
work status, income (Jindrová & Labudová, 2020; Shields &
Shooshtari,
2001) and even social capital (Carpiano, 2007; Dahl &
Malmberg-Heimonen, 2010). In this theoretical context, empirical pre-pandemic studies showed how
perceived
(and therefore, also actual) health is socially conditioned. From a micro-social perspective, perceived
health
is linked to age and sex - women and the elderly generally tend to report worse health status than men and
younger people - but also to work status, education and income -unemployed, with lower education and poor
subjects report worse health. From a macro-social viewpoint, previous studies proved the relationship
between
perceived health and different structural issues, like social policies (Fornell et al.,
2018), social inequality (Bobak et al., 2000), economic development (Olsen & Dahl, 2007) and economic crisis (Clair et al., 2016).
However, the outbreak of COVID-19 and the lockdown policies implemented to defeat it
completely redefined the social landscape. Mobility restrictions, social distancing measures and a new
fear of
contagion reframed the macro-social context in which people experience their health. At the same time, the
micro-context of individual resources and restrictions increased existing inequalities, producing new
situations, practices and problems that affect both feelings and perceptions (Duque-Calvache
et
al., 2021).
Most of the literature on the global effect of the lockdown on health perception has
shown a
generally negative trend. Lockdown measures have been found to increase mental problems like depression,
anxiety
and even suicidality (Rossi et al., 2020; Fountoulakis et al.,
2021).
Furthermore, authors measuring self-reported health conclude that people tend to assess their health as
significantly worse during lockdown than before (Ohlbrecht & Jellen, 2021).
However, most
of these studies do not compare 2020 data with independent data from the pre-pandemic situation, but
rather
retrospectively ask people about their health before and during lockdown. This type of comparison tends to
create an automatic discourse in respondents, due to their exposure to a large number of opinions
regarding the
effects of the lockdown on their social environment. Moreover, there is not enough evidence to prove a
general
worsening in perceived health. In fact, the only study found that compares perceived health during the
lockdown
with pre-pandemic data (Recchi et al., 2021) shows the opposite: an overall improvement in perceived
health and
well-being. The authors call this trend the ‘eye of the hurricane paradox’, an overrated self-perceived
health
amongst the uninfected. In other words, by comparing themselves with those infected with COVID-19, people
self-assess their health better than they would in a different context.
However, beyond this debate, most studies agree about the uneven effects of the
lockdown on
different social groups. These consequences are intertwined with classic socio-demographic (age and sex),
socio-economic (work status, income and educational level) and residential (housing and residential
environment)
determinants of perceived health. Regarding age, the lockdown seems to have reversed the typical trend, in
that
young people appear to be more seriously affected, particularly in psychological terms (Fiorenzato et al., 2021; Szwarcwald et al., 2021) due to the greater
impact
of the lockdown on young people’s daily routines (Fiorenzato et al., 2021) and their
greater
exposure to the virus (Mao et al., 2021). Women also appear to have experienced a
decrease in
perceived health, widening pre-existing gender inequalities (Broche-Pérez et al., 2021;
Elran-Barak & Mozeikov, 2020). The gendered division of domestic labour, especially
regarding caring duties, is the most likely cause for this trend (Brigidi et al., 2021).
For
socio-economic dimensions, the studies have confirmed the continuity of pre-2020 trends: respondents who
are
unemployed (Smith et al., 2020; Fiorenzato et al., 2021), poor (Szwarcwald et al., 2021) and/or with lower education (Elran-Barak &
Mozeikov, 2020; Ohlbrecht & Jellen, 2021) feel worse in physical and mental
terms
in the lockdown. With regard to residential conditions, evidence is scarce, with only a few studies
considering
housing variables. In general, those studies observe how living in smaller dwellings (Poortinga
et al., 2021) or in high-density residential environments (Recchi et al., 2020)
lowers
health perception, mainly the psychological aspect. It has also been found that the availability of
gardens or
open spaces protects against these effects (Noël et al., 2021).
Finally, evidence related to the connection between perceived health and changes in
everyday
life due to the lockdown is even more limited and usually focuses on physical exercise, consumption habits
(drugs, alcohol and food) and direct contact with COVID-19. Exercising has been found to be a protective
factor
(Cheval et al., 2021), and is even highlighted in some studies as the most important
determinant of perceived health during lockdown (Eder et al., 2021). However, most of
the
population exercised less frequently during lockdown (Mesa-Pedrazas et al., 2021).
Meanwhile,
significant increases in unhealthy behaviours such as smoking and drinking were detected (Niedzwiedz et al., 2021; Szwarcwald et al., 2021), with negative
effects on
perceived health, especially in terms of mental health. Contact with the COVID-19 disease is also a main
determinant of self-reported health. The death of relatives or friends due to COVID-19, direct exposure to
the
disease, personally knowing infected people or even living in regions with a high incidence of the disease
lowered perceived health (Rossi et al., 2020; Mao et al., 2021).
Although
those changes are crucial to explain perceived health, other relevant phenomena have not yet been studied,
such
as changes in the composition of households, distance from family networks and cohabitation conflicts.
Indeed,
previous studies have shown how family was one of the major concerns during the pandemic (Mesa-Pedrazas et
al.,
2021), as many people decided to move to be close to their relatives (Duque-Calvache et al.,
2021). Economic problems arising from the lockdown have also been found to be important. Situations
such
as being fired or furloughed from one’s job (Smith et al., 2020), a reduction of income
(Pieh et al., 2020) and non-payment of housing rent and supplies (Rogers
&
Power, 2020) are also relevant factors in understanding changes in self-reported health.
DATA AND METHODS
The main data source used in this paper is the 2020 Social Survey. Habits and
Living
Conditions of the Andalusian Population during the State of Alarm (IECA, 2020).
The
fieldwork was carried out between 15 April and 29 May 2020, and responses were collected from 2,950
individuals
from all 8 provinces in Andalusia. This survey was selected for three main reasons: (1) its timing, as it
covers
the period from the end of the strict lockdown phase to the beginning of the de-escalation phases; (2) it
is the
only publicly available source in Andalusia that contains information on perceived health during the most
restrictive phase of the pandemic and asks separately about self-reported global health and mental health;
(3)
the questionnaire contains a large number and wide diversity of variables, ranging from very detailed
indicators
on social and housing conditions and daily activities to contact with the disease in different social
circles,
making it possible to construct more complex models that include different possible explanations for
self-reported health.
In addition to this main source, the 2019 European Union Statistics on Income and
Living
Conditions (EU-SILC) dataset for Spain (INE, 2020) was also analysed,
using only
the sub-sample for Andalusia. This provided a benchmark to compare the results of the 2020 Social
Survey
with independent, pre-pandemic data on self-reported health. There is no doubt that this is the most valid
measurement of the changes brought by the lockdown measures on overall population health perception and on
the
effects of socio-demographic, socio-economic and residential determinants. The 2019 EU-SILC dataset
includes a question about self-perceived health (the main dependent variable) and many questions about
individual determinants that parallel the information available in the 2020 Social Survey. Given
the huge
sample size of the EU-SILC, even the Andalusian sub-sample is statistically representative,
providing a
solid measurement for the situation prior to the COVID-19 outbreak.
Data analysis was done in three main stages. In the first stage, the study compared
overall
self-perceived health scores in the 2019 EU-SILC and 2020 Social Survey to assess the impact
of
the lockdown measures on health perceptions. In the second stage, socio-demographic, socio-economic and
residential determinants of perceived health were analysed, both before and during lockdown. To do so, two
logit
models were developed to predict overall perceived health. The five categories of the original variable
were
recoded into one simple binary measure: 1 = ‘Has good or very good health’ and 0 = ‘Has average, bad or
very bad
health’. This decision was taken not only to simplify the analyses, but also to reflect the common way of
thinking about health amongst the population (which is closer to a good-bad binomial choice than to the
scale
used by the questionnaires). The model also includes a set of independent variables, including having a
chronic
health condition, age, sex, household composition, education, work status, income, housing type and
residential
environment. To compare the pre- and post-pandemic models, the study used Average Marginal Effects (AMEs),
a
strategy advocated by Williams (2012) to compare logit models calculated over different
samples. The comparison serves two main purposes: first, to contrast the general adjustment of the models,
measured as pseudo-R², in order to know the extent to which the independent variables selected explain
perceived
health in pre-pandemic and lockdown contexts; and second, to examine the significance and magnitude of the
AMEs,
to discover whether the effect of each variable changed during the lockdown. Finally, the goal of the
third
stage is to understand how different social changes directly caused by the lockdown have affected people’s
overall health self-perception, and the specific effect on self-reported mental health. To this end, two
stepwise logit models were developed, one for perceived overall health, and a second one for perceived
mental
health (in both models, the dependent variables are defined as a binary of good or bad health). In the
first
step, only individual determinants conventionally employed in self-rated health studies were used. In the
second
one, additional variables reporting social changes caused by the lockdown were added. These
lockdown-specific
variables include contact with the disease, increase in certain habits (particularly sleeping, drinking
and
smoking), frequency of physical exercise and reading during confinement, number of weekly trips, changes
in
household composition, emergence of cohabitation problems, economic problems (including the Spanish
temporary
layoff regulation known as ERTE, housing default, supply default and expected income reduction) and two
variables not directly related to confinement, but which became particularly significant during the
lockdown:
Internet access and having sufficient natural light. The paper reports the change in the overall
adjustment
statistics of the model as Akaike Criterion (AIC), Bayesian Information Criterion (BIC) and Pseudo-R² (Escobar et al., 2009) to quantify the effect of the lockdown measures and changes.
Finally,
the study compares the individual determinants that explain self-rated general and mental health (again,
based
on the use of AMEs).
RESULTS. EFFECTS OF MATERIAL CONDITIONS AND SOCIAL CONTEXT ON SELF-REPORTED HEALTH
Lockdown impact on self-reported health
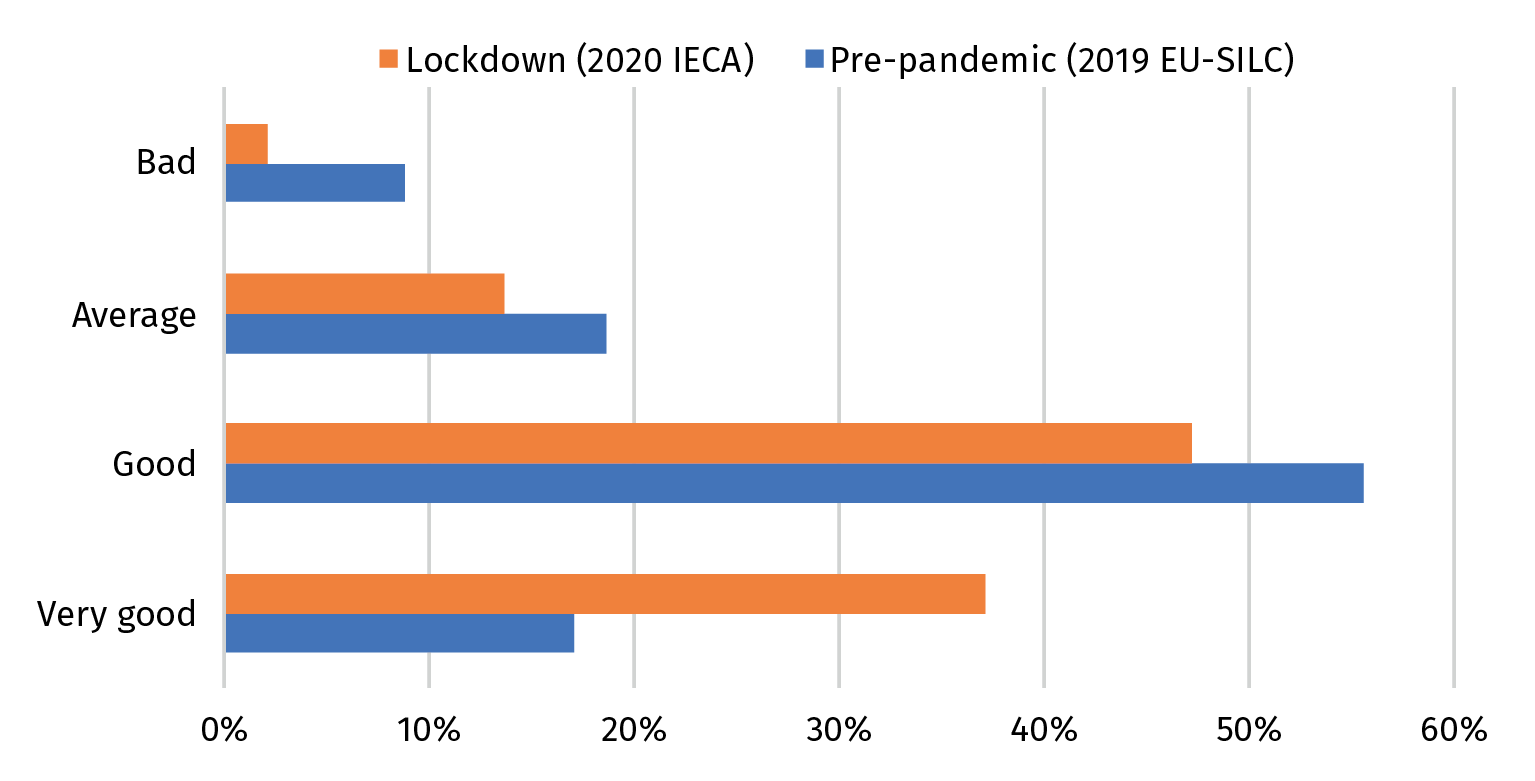
The predominant fact about the self-reported health of the Andalusian population as
a
result of the pandemic outbreak is the noticeable improvement over the 2019 situation, as seen in Figure 1. This result echoes the findings of Recchi et al. (2020) as
opposed to the opinion expressed by Ohlbrecht & Jellen (2021). In a context of
social
alarm and general concern, people tend to feel healthier (as long as they are not suffering from the
effects
of the COVID-19 illness), and at both ends of the scale: fewer people report poor health; more people
report a
very good situation. Social discourses on the gravity of the crisis permeate the respondents’
self-perception,
and their assessment is built on a relative definition of health. In other words, if others are
suffering
more, then their health may not merit a complaint.
Figure 1. Self-reported overall health before and during lockdown
Source: 2020 Social Survey. Habits and Living Conditions of the Andalusian Population during
the
State of Alarm (IECA, 2020) and EU-SILC 2019 for Spain (INE,
2020).
The sensitivity of the main variable to the context could be seen as a weakness, as
it is
not very closely connected to objective health conditions. However, the relative nature of the variable
is a
strong point, as it reflects how people feel about themselves. This self-assessment forms the basis of
their
behaviour: people decide to go to the doctor or to take medication, for example, based on how they feel.
Of
course, these decisions can be mistakes, and some reports (Woolf et al., 2021)
observe an
increase in mortality due to delayed care or the inadequate treatment of diseases different than
COVID-19.
1
This first finding has a clear practical implication: exposure to a lot of information on a single
disease clearly increases awareness on that particular threat but distracts attention on other
conditions the
subjects may suffer. Respondents think of themselves as healthy as long as they have no COVID-19, and
the
public messages about avoiding going to medical centres reinforce this wrong assumption.
Table 1. Percentages of respondents reporting ‘good’ or ‘very good’ overall health in
different social
categories before and during the lockdown
|
|
Pre-pandemic (2019 EU-SILC) |
Lockdown (2020 IECA) |
Difference |
|
Age group |
|
|
|
|
<30 |
95% |
93% |
-3% |
|
30-39 |
94% |
93% |
-1% |
|
40-49 |
83% |
89% |
6% |
|
50-65 |
67% |
80% |
14% |
|
66-74 |
52% |
70% |
19% |
|
>74 |
31% |
63% |
32% |
|
Has a chronic illness |
|
|
|
|
No |
93% |
91% |
-1% |
|
Yes |
30% |
70% |
40% |
|
Sex |
|
|
|
|
Male |
76% |
88% |
13% |
|
Female |
70% |
81% |
11% |
|
Household type |
|
|
|
|
One-person household |
55% |
74% |
19% |
|
Family |
75% |
86% |
10% |
|
Other households |
73% |
82% |
8% |
|
Education level |
|
|
|
|
No education |
40% |
65% |
24% |
|
Primary |
54% |
72% |
18% |
|
Secondary |
77% |
84% |
7% |
|
A-levels / Vocational training |
84% |
88% |
4% |
|
University degree |
87% |
91% |
4% |
|
Work status |
|
|
|
|
Worker |
89% |
91% |
2% |
|
Business owner / Self-employed |
83% |
91% |
8% |
|
Unemployed |
79% |
86% |
6% |
|
Inactive |
55% |
76% |
20% |
|
Monthly household income (in Euros) |
|
|
|
|
450 or less |
78% |
76% |
-2% |
|
451-900 |
60% |
76% |
16% |
|
901-1600 |
64% |
84% |
20% |
|
1601-2500 |
75% |
87% |
12% |
|
2501 or more |
80% |
94% |
14% |
|
Housing type |
|
|
|
|
Flat or other |
73% |
84% |
11% |
|
Detached home |
73% |
85% |
12% |
|
Residential environment |
|
|
|
|
High-density |
72% |
84% |
12% |
|
Medium density |
76% |
85% |
9% |
|
Low-density |
71% |
82% |
11% |
|
Total |
73% |
84% |
12% |
However, this improvement in self-reported health does not affect all social groups
equally. To verify this finding, we calculated the percentages of respondents reporting ‘good’ or ‘very
good’
overall health in different social categories. Table 1 shows a general upwards trend
across
all the social groups, but an even bigger increase in some of the categories with lower self-reported
health
before COVID-19: those affected by chronic conditions, people living alone, respondents with lower
education
and non-active individuals. On the other hand, among younger respondents, those with a low income and
individuals with no existing illness, there was a downwards change in their overall self-perceived health.
The
results for the first two groups were predictable. Young respondents (under 40) experienced a more extreme
change in their daily routines due to lockdown restrictions, while the poor (those earning less than €450)
experienced distress due to economic uncertainty, which will be further explored in the section on mental
health. The negative effect on individuals with no existing illness is also connected to the limitations
imposed by the lockdown on a population unaccustomed to having restrictions in their lives (unlike
individuals
with chronic illnesses).
With most of the variables, the differences between the categories decreased as a
result
of the pandemic; in other words, the restrictions had an equalizing effect. Only two variables show an
increase in differences: sex (the gap between women and men widened) and income (the gap between rich and
poor
also grew). With regard to the latter, it is notable that, while this difference did not have a clear
effect
on self-perceived health before the crisis, the trend is easy to identify during the lockdown. Therefore,
apart from all the lives lost and the economic mayhem, the pandemic brought an increase in the inequality
of a
society that was already uneven.
Changes in the determinants of perceived health in the lockdown
Regarding the second goal —to discover how demographic, socio-economic and residential
conditions explain health self-perception and whether these conditions have changed due to the pandemic—
two
different logit regressions were used to compare the effects (before and during the lockdown) of the
different
variables usually included in overall self-reported health models. As the models use information from
different datasets, with different variances, AMEs are included in the table instead of the usual
coefficients/odds ratios. The main advantage of these models over the descriptive statistics used in the
previous section is the isolation of the effect of each variable (while controlling the other variables),
which makes it possible to separate and identify their individual relevance. The results, which are
noteworthy
in a number of ways, are presented in Table 2.
The first outstanding result is the breakdown of the explanatory power of the classic
predictors of self-reported health in a pandemic context. The pseudo-R2 plummets from
explaining
48% of the variance to a meagre 15% in 2020. It is much more difficult to explain self-perception of
health
during the lockdown, either the feeling is connected to social variables not included in this attempt, or
maybe it is explained by personal or even psychological features of the subjects. These results convinced
us
to create separate models for overall health and mental health (see next section), in order to study the
importance of non-physical well-being and its connection with the lockdown situation.
In 2019, the link between objective and subjective health was quite strong (chronic
conditions were the most powerful predictors). The rest of the variables worked as expected after reading
the
literature. But in the 2020 model, some variables lost explanatory power, ceased to be significant while
others increased their power or began to create significant differences. The most important addition to
the
previous model was the sudden appearance of income as an explanatory indicator of overall health. In a
publicly funded, universal healthcare society —with some exceptions related to rare conditions and
treatments—
money made very little difference in self-reported health before the pandemic, which undoubtedly was a
success
of the system. However, after the arrival of COVID-19, income became important, and its effect is linear
to
wellbeing. This is a very important finding with strong political implications: the pandemic has opened a
new,
worrisome, breach between the perceived health of the rich and the poor. To compensate these social
differences will require additional resources and a determined intervention in the health system, if we
want
to reach pre-pandemic levels of well-being.
Table 2. Average Marginal Effects of the variables on overall self-reported health before and
during
lockdown
|
|
Pre-pandemic (2019 EU-SILC) |
|
|
Lockdown (2020 IECA) |
|
|
|
|
dy/dx |
Sig |
SE |
dy/dx |
Sig |
SE |
|
Has a chronic illness (Ref: No) |
-28.3% |
*** |
0.006 |
-13.8% |
*** |
0.014 |
|
Age |
-1.0% |
*** |
0.002 |
-0.5% |
* |
0.002 |
|
Age squared |
0.0% |
** |
0.000 |
0.0% |
|
0.000 |
|
Sex (Ref: Male) |
|
|
|
|
|
|
|
Female |
-2.4% |
* |
0.012 |
-5.9% |
*** |
0.014 |
|
Household type (Ref: Family) |
|
|
|
|
|
|
|
One-person household |
-1.4% |
|
0.022 |
-0.6% |
|
0.025 |
|
Other households |
-3.0% |
* |
0.013 |
-2.4% |
|
0.019 |
|
Educational level (Ref: Secondary) |
|
|
|
|
|
|
|
No education |
-4.2% |
* |
0.017 |
-6.0% |
* |
0.026 |
|
Primary |
-2.6% |
|
0.017 |
-3.1% |
|
0.022 |
|
A-levels / Vocational training |
3.4% |
* |
0.017 |
0.2% |
|
0.019 |
|
University degree |
5.5% |
** |
0.020 |
1.9% |
|
0.025 |
|
Work status (Ref: Inactive) |
|
|
|
|
|
|
|
Worker |
4.6% |
** |
0.017 |
3.7% |
|
0.021 |
|
Business owner / Self-employed |
0.8% |
|
0.025 |
2.5% |
|
0.033 |
|
Unemployed |
2.4% |
|
0.017 |
0.3% |
|
0.022 |
|
Monthly household income (in Euros) (Ref: 2501 or more) |
|
|
|
|
|
|
|
450 or less |
-1.0% |
|
0.034 |
-11.9% |
** |
0.041 |
|
451-900 |
-4.1% |
|
0.023 |
-9.7% |
** |
0.030 |
|
901-1600 |
-2.2% |
|
0.019 |
-8.0% |
** |
0.029 |
|
1601-2500 |
-0.7% |
|
0.016 |
-7.7% |
** |
0.030 |
|
No response |
|
|
|
-6.9% |
* |
0.033 |
|
Housing type (Ref: Flat or other) |
|
|
|
|
|
|
|
Detached home |
0.9% |
|
0.013 |
1.7% |
|
0.015 |
|
Residential environment type (Ref: Medium density) |
|
|
|
|
|
|
|
High-density |
-0.2% |
|
0.016 |
0.4% |
|
0.016 |
|
Low-density |
-1.6% |
|
0.016 |
-1.1% |
|
0.023 |
|
N |
4,051 |
|
|
2,948 |
|
|
|
Pseudo R² |
0.48 |
|
|
0.15 |
|
|
|
*p-value<0.05; **p-value<0.01; ***p-value<0.001 |
|
|
|
|
|
|
Self-reported health and its connection with life in lockdown
Given that the classic predictors do not explain perceived health in a pandemic
context,
in the midst of severe restrictions on mobility and everyday behaviour, the next logical step was to
include
some of these changes as independent variables in the models. Spending the majority of their time inside
their
homes required a remarkable effort on the part of all individuals to adjust their routines and usual
priorities. Although some people were able to withstand (and even to enjoy) the situation, for others the
changes came at a price, especially in emotional terms. While the previous sections analysed overall
self-reported health, this one focuses on both the general assessment of health and also specific measures
of
mental health, as presented in Table 3. Mental health is harder to explain by social
factors, as it is related to personal experiences, personality traits and the way people interact with the
environment. In fact, the variables that explained almost 50% of the variance in overall health before
COVID-19 (and 15% after it appeared) are mostly unrelated to mental health (the R2 is 0.05, a
very
poor model).
When the new variables are included, the models improve in all the measures (Akaike
and
Bayesian criteria, pseudo-R2 and log-likelihood). However, the improvement in mental health is
clearly more significant, as it doubles the explanatory power of the previous step in the model, and
especially because most of the variables have significant effects on the dependant variable. It is hard to
pinpoint why one person may feel better or worse in terms of mental health (thus most of the variance
remains
unexplained), but it is clear that the lockdown measures affected mental health in a way unparalleled with
the
effect on general health. This fact is coherent with some results found using different methodological
approaches compiled in the book by Del Campo Tejedor (2021). Staying at home limited our
physical activity, but our weak spot during the confinement period was our mind.
Although having a connection to the Internet at home was not related to the pandemic
situation per se, the possibilities it opens for those staying at home (either related to communication,
telework, entertainment or shopping) required its inclusion in the models. While it does not increase
mental
health, it positively affects general health. Having natural light at home, sleeping more and exercising
more
frequently are also variables with a stronger effect on general than on mental health (although they all
also
improve the latter). These findings are coherent with the literature. For the other variables, the effect
on
mental health is always stronger and more significant.
Everyday behaviours such as sleeping patterns and healthy/unhealthy habits are
significant
in the mental health model, although interpreting the results can be tricky. All these practices can be
considered not only factors producing lower mental health, but also consequences of that state of mind. Martínez-de-Quel et al. (2021) underline how lockdown measures specially affected the
sleep
patterns and eating habits of young, physically active population (previously inactive respondents in
their
study did not show the same effect). Mental sequels appear therefore to be related to the number of
changes in
our daily routine introduced by the restrictions, benefiting those who had a sedentary, inactive
lifestyle.
Table 3. Stepwise logit models to explain self-reported overall and mental health during
lockdown (expressed in
Average Marginal Effects)
|
|
|
|
Self-reported overall health |
|
|
|
|
|
Self-reported mental health |
|
|
|
|
|
Step 1 |
|
|
Step 2 |
|
|
Step 1 |
|
|
Step 2 |
|
|
|
|
dy/dx |
Sig |
SE |
dy/dx |
Sig |
SE |
dy/dx |
Sig |
SE |
dy/dx |
Sig |
SE |
|
Has a chronic illness (Ref: No) |
-13.8% |
*** |
0.01 |
-13.5% |
*** |
0.01 |
-5.4% |
** |
0.02 |
-5.1% |
** |
0.02 |
|
Age |
-0.5% |
* |
0.00 |
-0.4% |
|
0.00 |
0.4% |
|
0.00 |
0.4% |
|
0.00 |
|
Age squared |
0.0% |
|
0.00 |
0.0% |
|
0.00 |
0.0% |
|
0.00 |
0.0% |
|
0.00 |
|
Sex (Ref: Male) |
|
|
|
|
|
|
|
|
|
|
|
|
|
Female |
-5.9% |
*** |
0.01 |
-5.3% |
*** |
0.01 |
-8.8% |
*** |
0.02 |
-8.5% |
*** |
0.02 |
|
Household type (Ref: Family) |
|
|
|
|
|
|
|
|
|
|
|
|
|
One-person household |
-0.6% |
|
0.02 |
-0.3% |
|
0.02 |
-2.9% |
|
0.03 |
-3.0% |
|
0.03 |
|
Other households |
-2.4% |
|
0.02 |
-2.4% |
|
0.02 |
-2.8% |
|
0.02 |
-2.9% |
|
0.02 |
|
Educational level (Ref: Secondary) |
|
|
|
|
|
|
|
|
|
|
|
|
|
No education |
-6.0% |
* |
0.03 |
-3.0% |
|
0.03 |
-11.0% |
*** |
0.03 |
-7.5% |
* |
0.03 |
|
Primary |
-3.1% |
|
0.02 |
-2.0% |
|
0.02 |
-5.5% |
* |
0.02 |
-4.3% |
|
0.02 |
|
A-levels / Vocational training |
0.2% |
|
0.02 |
-0.7% |
|
0.02 |
-0.9% |
|
0.02 |
-2.2% |
|
0.02 |
|
University degree |
1.9% |
|
0.03 |
-0.7% |
|
0.03 |
4.2% |
|
0.03 |
1.0% |
|
0.03 |
|
Work status (Ref: Inactive) |
|
|
|
|
|
|
|
|
|
|
|
|
|
Worker |
3.7% |
|
0.02 |
5.1% |
* |
0.02 |
-0.5% |
|
0.02 |
2.4% |
|
0.02 |
|
Business owner / Self-employed |
2.5% |
|
0.03 |
3.6% |
|
0.03 |
2.5% |
|
0.03 |
5.0% |
|
0.03 |
|
Unemployed |
0.3% |
|
0.02 |
1.7% |
|
0.02 |
-2.0% |
|
0.02 |
1.1% |
|
0.02 |
|
Monthly household income (in Euros) (Ref: 2,501 or higher) |
|
|
|
|
|
|
|
|
|
|
|
|
|
450 or less |
-11.9% |
** |
0.04 |
-8.5% |
* |
0.04 |
-4.3% |
|
0.04 |
-0.6% |
|
0.04 |
|
451-900 |
-9.7% |
** |
0.03 |
-8.0% |
** |
0.03 |
-7.2% |
* |
0.03 |
-4.9% |
|
0.03 |
|
901-1600 |
-8.0% |
** |
0.03 |
-7.0% |
* |
0.03 |
-6.6% |
* |
0.03 |
-5.1% |
|
0.03 |
|
1601-2500 |
-7.7% |
** |
0.03 |
-7.6% |
** |
0.03 |
-2.8% |
|
0.03 |
-2.7% |
|
0.03 |
|
No response income |
-6.9% |
* |
0.03 |
-6.1% |
|
0.03 |
-4.0% |
|
0.03 |
-3.5% |
|
0.03 |
|
Housing type (Ref: Flat or other) |
|
|
|
|
|
|
|
|
|
|
|
|
|
Detached home |
1.7% |
|
0.01 |
1.3% |
|
0.01 |
2.0% |
|
0.02 |
1.7% |
|
0.01 |
|
Residential environment type (Ref: Medium-density) |
|
|
|
|
|
|
|
|
|
|
|
|
|
High-density |
0.4% |
|
0.02 |
0.3% |
|
0.02 |
-0.6% |
|
0.02 |
-0.6% |
|
0.02 |
|
Low-density |
-1.1% |
|
0.02 |
-0.5% |
|
0.02 |
-5.5% |
* |
0.02 |
-5.5% |
* |
0.02 |
|
Has internet (Ref: No) |
|
|
|
5.0% |
* |
0.02 |
|
|
|
5.4% |
|
0.03 |
|
Has enough natural light (Ref: No) |
|
|
|
9.6% |
** |
0.03 |
|
|
|
9.2% |
** |
0.03 |
|
Personally knows people with COVID (Ref: No) |
|
|
|
-1.2% |
|
0.02 |
|
|
|
-3.8% |
* |
0.02 |
|
Increased alcohol consumption (Ref: No) |
|
|
|
1.1% |
|
0.03 |
|
|
|
-8.2% |
** |
0.03 |
|
Increased smoking habit (Ref: No) |
|
|
|
-3.8% |
|
0.02 |
|
|
|
-8.4% |
*** |
0.02 |
|
Increased sleeping time (Ref: No) |
|
|
|
8.5% |
** |
0.03 |
|
|
|
8.4% |
** |
0.03 |
|
Weekly exercise frequency |
|
|
|
1.0% |
*** |
0.00 |
|
|
|
0.7% |
** |
0.00 |
|
Weekly reading frequency |
|
|
|
0.4% |
|
0.00 |
|
|
|
1.0% |
*** |
0.00 |
|
Number of weekly trips |
|
|
|
0.1% |
|
0.00 |
|
|
|
0.2% |
|
0.00 |
|
Changes in household composition (Ref: No) |
|
|
|
4.3% |
|
0.03 |
|
|
|
0.4% |
|
0.03 |
|
Cohabitation problems (Ref: No) |
|
|
|
-0.8% |
|
0.03 |
|
|
|
-11.3% |
*** |
0.03 |
|
Housing default (Ref: No) |
|
|
|
-5.4% |
|
0.03 |
|
|
|
-2.2% |
|
0.03 |
|
Supply default (Ref: No) |
|
|
|
-4.6% |
|
0.02 |
|
|
|
-5.5% |
* |
0.03 |
|
Expected income reduction (Ref: No) |
|
|
|
-1.8% |
|
0.01 |
|
|
|
-4.6% |
** |
0.01 |
|
Paid leave (Ref: No) |
|
|
|
1.0% |
|
0.03 |
|
|
|
0.6% |
|
0.03 |
|
N |
2,948 |
|
|
2,948 |
|
|
2,938 |
|
|
2,938 |
|
|
|
Pseudo R² |
0.15 |
|
|
0.18 |
|
|
0.05 |
|
|
0.10 |
|
|
|
AIC |
1,808 |
|
|
1,741 |
|
|
2,110 |
|
|
2,004 |
|
|
|
BIC |
5,306,054 |
|
|
5,109,207 |
|
|
6,176,563 |
|
|
5,865,836 |
|
|
|
Log-Lik |
-2,665,000 |
|
|
-2,566,000 |
|
|
-3,100,000 |
|
|
-2,945,000 |
|
|
Regarding the variables linked to social interaction, knowing people who suffered
through
COVID-19 has an effect on mental health, as observed by Rossi et al. (2021). Unexpectedly, the number of
times
a person left their home during a week does not have any statistical connection with overall or mental
health.
Again, is this a cause or a consequence? Were people staying at home because they were worried, scared or
feeling unwell? Was going out a healthy activity at the time? The diversity of situations and
contradictory
reasons to stay or go out are probably blurring any significant effect of the variable. Changes in
household
composition were not affecting wellbeing, although it has been argued that most changes in the households
were
in reaction to housing or care needs (Duque-Calvache et al., 2021). Residential mobility
may
have spared some households from further problems, but that effect is diluted in this sample. Spending
more
time at home increased the chances for cohabitation conflicts, and the connection of these problems with a
decrease in mental health is clear.
Finally, indicators of economic problems resulting from the pandemic explain a loss of
self-reported mental health. It has been shown that financial hardship is connected to anxiety levels and
therefore directly affects emotional wellbeing, but not physical health. Of course, given that the survey
was
conducted during the early stage of the pandemic, most of the mid- and long-terms effects of the social
and
economic crisis had yet to manifest themselves. The effects of a sudden, shocking and persistent change in
all
the aspects of a life will have to be studied along the next years, with special attention to children and
their coping strategies (Orgilés et al., 2021).

![]()

![]()

![]()